Masters of Denial
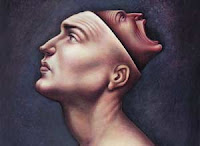 As far as these patients are concerned,the problem is yours, not theirs.
As far as these patients are concerned,the problem is yours, not theirs.It has got so psychologist Lawrence Josephs can tell right away which patients are likely to fire him. The narcissists may be the worst. These are the ones who are there in the first place only because their spouse would not quit hectoring them to show more interest in the marriage, and the people at work just didn’t seem to give them the credit or attention they deserve. Often, they stay only long enough to decide that what they really need is to leave the marriage and quit the job. After that, they sack the shrink. “They come in under duress:’ says Josephs, a psychology professor at Adelphi University in Garden City N.Y. “But they don’t commit. What they really want is to have everything on their own terms
If it’s any comfort to Josephs, he’s not alone in having such trouble managing nar- cissists—and it’s not just the narcissists giving therapists such problems. Narcissism is one of 10 conditions under the diagnostic heading of personality disorders (PD), and by most accounts, narcissists are among psychology’s toughest nuts to crack. Talk therapy often doesn’t touch them; drug therapy may do just as little. Researchers know why. Common mental conditions, such as anxiety disorders, eating disorders and depression, can be thought of as a pathological rind wrapped around an intact core. Peel the skin away through talk therapy or melt it away with drugs, and the problem may abate. Personality disorders, by contrast, are marbleized through the entire temperament. Narcissists may be self-absorbed, but they believe they jolly well have a right to be. Histrionic personalities may make too much of things, hut how else can they be heard? It’s hard enough to persuade most people to see a therapist—harder still when the patient denies there’s a problem at all. “People rarely come in with a self-diagnosed personality disorder,” says Josephs. “Friends and family push them into it.”
These days they have more reason than ever to push. As families increasingly frag- ment and as societal pressures grow, experts say they are seeing more cases of personality disorder than ever. As much as 9% of the population is thought to suffer from some kind of personality disorder, and as many as 20% of all mental-health hospitalizations may be the result of such conditions. Epidemiologists have not done a very good job of comparing these figures with those of earlier years, but many doctors report—anecdotally—that their PD caseload is indeed on the rise. “The more severe ones are increasing:’ says Josephs, “especially among people who grew up in homes with divorce or drug and alcohol problems.”
As this happens, more and more researchers are looking for new ways to treat the conditions—exploring both genetic and environmental roots, seeking both thera- peutic and chemical cures. And well they might. “The social costs of personality disorders are huge:’ says Dr. John Gunderson, director of the Personality Disorders Service at McLean Hospital in Belmont, Mass. “These people are involved in so many of society’s ills—divorce, child abuse, violence. The problem is tremendous.” While solutions are elusive, the pathological arc of PDs is predictable. They tend to show up after age 18, striking men and women equally—though gender may influence which of the 10 disorders a person develops. The disorders are grouped into three subcategories, and of these, the so called dramatic cluster—borderline, antisocial, narcissistic and histrionic disorders—is the best known. But it’s the borderlines who cause doctors—to say nothing of families—the most headaches.
People with borderline-personality disorder form exceedingly volatile relationships, whipsawing between idealizing family and friends and dismissing them as worth- less or hateful. They are intensely afraid of being abandoned but react so savagely when a loved one disappoints them that abandonment is often just what they get. Prod these people into therapy, and the same dynamic unfolds there. “At one point, you’re their closest friend, and two weeks later, you’re the enemy,” says Norman Clemens, a psychology professor at Case Western Reserve University in Cleveland.
Histrionic and narcissistic personalities use drama or self-absorption in much the same way—pushing away family and exasperating therapists. People with antisocial personalities raise the stakes higher, exhibiting aggressiveness, lack of conscience and indifference to the law, often folding criminal behavior into their pathology. Less dramatic but just as stubborn is the so-called anxious cluster, including the straightforwardly named dependent personality, the socially withdrawn avoidant personality and the rigid and rule-bound obsessive-compulsive personality (a different diagnosis entirely from obsessive-compulsive disorder an anxiety condition). The third group—actually called the odd cluster—includes the paranoid, schizotypal and schizoid personalities. Paranoid sounds like just what it is. Schizotypals and schizoids both have problems forming relationships and interpreting social cues; schizotypals may also suffer delusions. “Schizoids are lone wolves:’ says Clemens. “Schizotypals skate along the edge of real schizophrenia’
Before scientists can figure out how to treat these conditions, they must first figure out what’s behind them. Few researchers doubt that when disorders are so woven into temperament, some of what causes them is written into genes. A Norwegian study published in 2000 examined identical and fraternal twins and found that matched pairs—with their matched genetic blueprints—were more likely to share personality disorders than unmatched pairs. The borderline personality had an estimated 69% level of inherit-ability This confirms the observations of doctors in the field who notice higher rates of personality disorders among descendants of PD sufferers. “There are almost certainly multiple genes involved in predisposing people to PD5,” says Gunderson.
But genes aren’t everything. Therapists who work with narcissists often uncover ~ childhood abuse or some other trauma leading to low self-esteem or even self-loathing—just the kind of emotional hole that pathological grandiosity would be designed to fill. Borderline-personality disorder affects more women than men, and some research has shown that up to 70% of borderline women were sexually or physically abused at some point in their lives. It’s hard to hang that kind of mistreatment on the genes. Poorly handled bipolar disorder or learning disabilities may also evolve into personality disorders. Dr. Larry Siever, professor of psychiatry at Mt. Sinai School of Medicine in New York City, believes that some of the rise in PDs may be linked to the loss of natural support groups, as individuals in an increasingly mobile culture migrate farther and farther from home. “In the past,” he says, “we lived close to our extended families in highly structured communities. People could take care of their own and rein them in:’
Whatever the specific roots of the conditions, once those environmental and genetic die are cast, is that it for the disordered personality? The short, bleak answer is of- ten yes—at least as long as PD patients resist acknowledging the problem. Anxiety disorders such as phobias are generally referred to as ego-dystonic illnesses: the suf
ferer acknowledges the problem and wants to do something about it. Personality disorders are ego syntonic: individuals believe that the drama, self-absorption and other traits that characterize their condition are reasonable responses to the way the world is treating them. That’s a hard patient to heal, but there is hope, and some of it starts in the pharmaceutical lab.
Researchers are finding that anti-psychotics can help alleviate paranoid, schizoid and schizotypal symptoms. A variety of drugs—including mood stabilizers, such as lithium and Depakote; anticonvulsants like Tegretol; and ssRls—may help control the impulsive element of the dramatic disorders. And while antidepressant and anti-anxiety medications do little to rejigger something as fundamental as personality, doctors find that if they prescribe the drugs to relieve the stress that comes with living so disordered a life, some motivated patients may then take on the harder work of talk therapy.
For those who do, the options are growing. Analytic therapy, which explores past traumas, can uncover the deeply rooted conflicts behind the conditions. More immediate results can be gained through cognitive and behavioral therapy, which teach coping skills. A new treatment known as dialectical behavior therapy, developed by clinical psychologist Marsha Linehan of the University of Washington, can teach borderlines to recognize the situations that trigger explosive feelings, helping them squelch a reaction before it erupts. “The first thing we teach is to get control of the behavior,” says Linehan. “After that, we work on feeling bettet” When patients commit to some form of therapy, even the doctors can be surprised. A study conducted by Gunderson and colleagues at Harvard, Yale, Columbia and Brown looked at borderline, avoidant, obsessive-compulsive and schizotypal patients and found that, after two years of treatments, including medication, psychotherapy, DBT or group and family therapy, they showed a 40% improvement. “That’s big news,” says Gunderson. “Nobody would have thought we’d get better than 15%.”
Forty percent, however~ still leaves 60% suffering, and researchers hope to tip that balance the other way. At Mt. Sinai, Siever is looking deeper into what makes people neurologically susceptible to Pds, studying the structure and function of the brain itself in order to determine which areas misfire in the course of the disorders as well as the role played by such neurotransmitters as serotonin and dopamine. Others are studying such possible causes as high levels of stress hormones in the womb or even poor nutrition during brain development. Understanding the biochemistry should make it easier to develop medications.
Until then, it will mostly be up to patients to deny the lie that the disorder tells—that there’s really nothing wrong with them—and make the therapeutic commitment necessary to fix things. “Nobody totally changes,” says Josephs. “But anyone can become more flexible and resilient. Anyone can make progress:’ That alone is already a better prognosis than most patients have had.
http://www.time.com/time/magazine/article/0,9171,1101030120-407276,00.html

<< Home